Aerodigestive Tract
The aerodigestive tract consists of the organs and tissues of the respiratory tract and the upper part of the digestive tract (Andrews, 2006). The aerodigestive tract includes the
- airway (pharynx and larynx),
- pulmonary tract (trachea, bronchi, and lungs), and
- upper digestive tract (esophagus).
Breathing and swallowing functions take place in the aerodigestive tract. Both tasks elicit a complex, coordinated biomechanical sequence of events designed to protect the airway during eating and drinking, while maintaining sufficient airflow for phonation (Coyle, 2010; Jadcherla, 2012; Robbins, 2011).
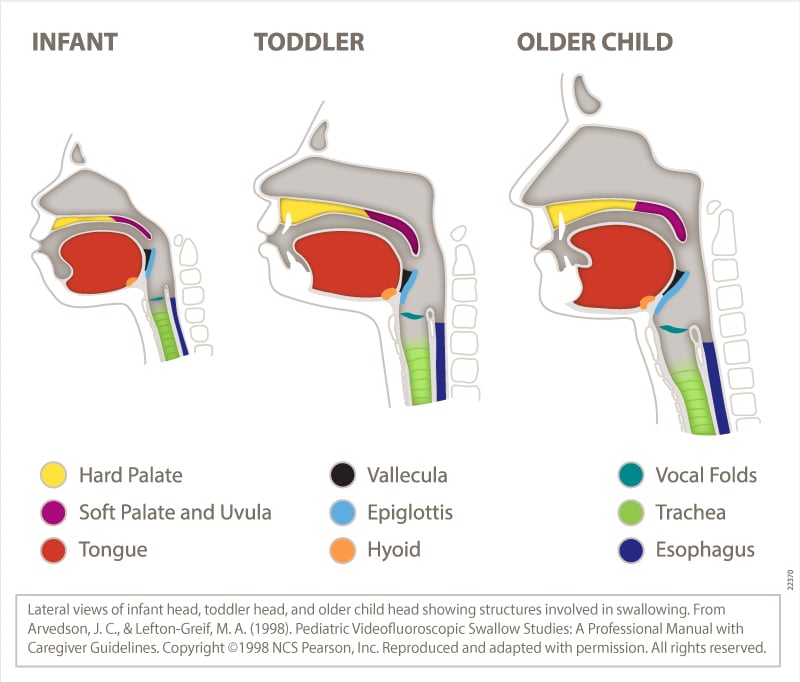
The aerodigestive anatomy and physiology of infants is different from that of adults (see figure below). These differences include the following:
- In infants, the tongue fills the oral cavity, and the velum (soft palate) is in close proximity to the epiglottis. The hyoid bone and the larynx are positioned higher in infants than in adults, and the larynx elevates less in infants than in adults during the pharyngeal phase of the swallow.
- Rapid suck–swallow sequences are characteristic of infant bottle-feeding and/or breastfeeding during sucking bursts. Precise coordination of sucking, swallowing, and respiration is essential for maintaining airway protection.
- The close proximity of oral structures and the sucking pads in the cheeks (in term infants) may provide positional stability to support efficient sucking action during bottle-feeding and breastfeeding.
- Once the infant begins eating pureed food (around 4–6 months), the oral and pharyngeal phases are similar to those of an adult (although with less elevation of the larynx).
- As the child matures, the intraoral space increases as the mandible moves downward and forward, and the oral cavity elongates in the vertical dimension. The space between the tongue and the palate increases, and the larynx and the hyoid bone descend, elongating and enlarging the pharynx (Logemann, 1998; Matsuo & Palmer, 2008).
Aerodigestive Disorders
Aerodigestive disorders are conditions or diseases of the aerodigestive tract—including the airway (pharynx and larynx), pulmonary tract (trachea, bronchi, and lungs), and upper digestive tract (esophagus)—that may affect respiratory and swallowing functions. Aerodigestive disorders, or the management of them (e.g. surgery, intubation), may result in voice, feeding, and/or swallowing problems as well as laryngeal airway problems—the term used in this Practice Portal page to refer to paradoxical vocal fold movement (PVFM) and chronic cough.
Aerodigestive disorders may be congenital, developmental, or acquired. They are not mutually exclusive—individuals may have more than one disorder (Jadcherla, 2012). In children, some aerodigestive disorders may resolve with maturity or with behavioral management, but others may require medical and/or surgical intervention.
Examples of common aerodigestive disorders (grouped by anatomical location) include, but are not limited to, the following:
Airway (Pharynx and Larynx)
- chronic cough
- dystussia
- epiglottitis
- fungal infections of the pharynx or the larynx (e.g., blastomycosis [rare], histoplasmosis, candidiasis)
- irritable larynx
- laryngeal clefts
- laryngeal or pharyngeal paralysis/paresis (unilateral or bilateral)
- laryngeal stenosis (supraglottic, glottic, or subglottic)
- laryngeal webs
- laryngomalacia (moderate to severe)
- laryngopharyngeal reflux
- laryngospasm
- muscle tension dysphagia
- muscle tension dysphonia
- PVFM
- breathing–swallowing incoordination (secondary to medical conditions such as chronic obstructive pulmonary disease (COPD), neurological insult, or head and neck cancer)
- structural or physiologic changes secondary to injury, neoplasms, radiation therapy, or surgery (e.g., pharyngeal or laryngeal resections, radiation for head and neck cancer treatment, prolonged intubation)
- velopharyngeal dysfunction
See Aerodigestive Disorders of the Airway (Pharynx and Larynx) [PDF].
Pulmonary Tract (Trachea, Bronchi, and Lungs)
- bronchomalacia
- chronic lung disease (e.g., asthma, emphysema, COPD)
- infectious diseases affecting pulmonary function (e.g., upper respiratory infection, pertussis [whooping cough], pneumonia, tuberculosis)
- neoplasms
- structural or physiologic changes affecting pulmonary function secondary to injury or surgery (e.g., pneumothorax [collapsed lung], pneumonectomy, lung transplantation)
- tracheal stenosis
- tracheoesophageal fistula
- tracheomalacia
See Aerodigestive Disorders of the Pulmonary Tract (Trachea, Bronchi, and Lungs) [PDF].
Upper Digestive Tract (Esophagus)
- esophageal motility disorder, including spasm and achalasia
- esophageal structural disorder, including stricture, web, diverticulum, and ring
- gastroesophageal reflux
- inflammatory forms of esophagitis (e.g., eosinophilic, viral, reflux-related)
See Aerodigestive Disorders of the Upper Digestive Tract (Esophagus) [PDF].
For detailed information about these and other aerodigestive disorders, see, for example, Andrews (2006), Ashland and Hersh (2009), Coyle (2010), Dinwiddie (2004), Jadcherla (2012), Matsuo and Palmer (2008), and Morris et al. (2006).
Speech-Language Pathologist (SLP) Involvement in Aerodigestive Disorders
Aerodigestive disorders can cause secondary problems in feeding, swallowing, voice, and/or laryngeal airway function. SLPs play a role in the screening, assessment, diagnosis, and treatment of these secondary problems and often work collaboratively with other professionals in providing services to individuals with aerodigestive disorders.
Paradoxical Vocal Fold Movement (PVFM)
Paradoxical vocal fold movement, or PVFM, is the intermittent, episodic adduction of the vocal folds during inspiration. During episodes, the vocal folds adduct partially or fully and restrict the passage of air to the lungs. PVFM can occur in isolation, or it can co-occur with other conditions, including pulmonary disorders (e.g., asthma), laryngeal abnormalities, and cardiac pathology (Reitz et al., 2014). About 29%–40% of those with PVFM also have asthma (Gurevich-Uvena et al., 2010). SLPs are involved in the diagnosis and direct behavioral management of PVFM.
Chronic Cough
Chronic cough is most commonly defined as a cough lasting more than 8 weeks in adults and more than 4 weeks in children (Asilsoy et al., 2008; Morice, 2004). Chronic cough may be termed “somatic cough syndrome” in the absence of a known cause or “tic cough” when it is accompanied by core clinical features of tics (e.g., suppressibility, distractibility, suggestibility, variability, and presence of a warning sensation; Vertigan, 2017). SLP intervention is an effective treatment for chronic cough (Gibson & Vertigan, 2009; Petty & Dailey, 2009) and addresses the management of cough regardless of the initiating cause.
.