Traumatic perforation of the tympanic membrane (TM) can cause pain, bleeding, hearing loss, tinnitus, and vertigo. Diagnosis is based on otoscopy. Treatment often is unnecessary. Antibiotics may be needed for infection. Surgery may be needed for perforations persisting > 2 months, disruption of the ossicular chain, or injuries affecting the inner ear.
Traumatic causes of tympanic membrane perforation include
-
Insertion of objects into the ear canal purposely (eg, cotton swabs) or accidentally
-
Concussion caused by an explosion or open-handed slap across the ear
-
Head trauma (with or without basilar fracture)
-
Longitudinal temporal bone fracture
-
Sudden negative pressure (eg, strong suction applied to the ear canal)
-
Barotrauma (eg, during air travel or scuba diving)
-
Iatrogenic perforation from instrumentation during irrigation or foreign body or cerumen removal
Penetrating injuries of the tympanic membrane may result in dislocations of the ossicular chain, fracture of the stapedial footplate, displacement of fragments of the ossicles, bleeding, a perilymph fistula from the oval or round window resulting in leakage of perilymph into the middle ear space, or facial nerve injury.
Symptoms and Signs of Traumatic TM Perforation
Traumatic perforation of the tympanic membrane causes sudden severe pain sometimes followed by bleeding from the ear, hearing loss, and tinnitus. Hearing loss is more severe if the ossicular chain is disrupted or the inner ear is injured. Vertigo suggests injury to the inner ear. Purulent otorrhea may begin in 24 to 48 hours, particularly if water enters the middle ear.
Diagnosis of Traumatic TM Perforation
Perforation is generally evident on otoscopy. Any blood obscuring the ear canal is carefully suctioned at low pressures. Irrigation and pneumatic otoscopy are avoided. Extremely small perforations may require otomicroscopy or middle ear impedance studies for definitive diagnosis (eg, if perforations do not close). If possible, audiometric studies are done before and after treatment to avoid confusion between trauma-induced and treatment-induced hearing loss.
Traumatic Perforation of Tympanic Membrane
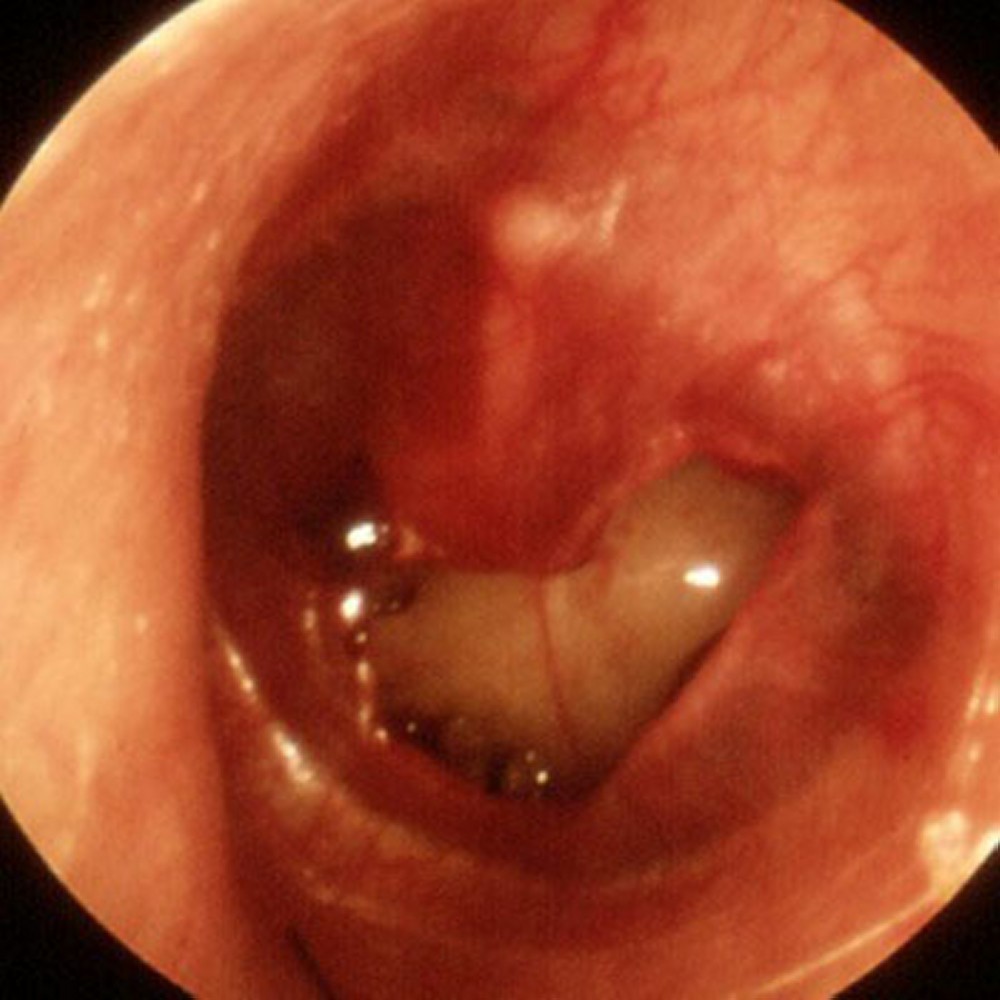
IMAGE PROVIDED BY PIET VAN HASSELT, MD.
Patients with marked hearing loss or severe vertigo are evaluated by an otolaryngologist as soon as possible. Exploration may be needed to assess and repair damage. Patients with a large tympanic membrane defect should also be evaluated, because the displaced flaps may need to be repositioned.
Treatment of Traumatic TM Perforation
Often, no specific treatment is needed. The ear should be kept dry; routine antibiotic ear drops are unnecessary. However, prophylaxis with oral broad-spectrum antibiotics or antibiotic ear drops is necessary if contaminants may have entered through the perforation as occurs in dirty injuries.
If the ear becomes infected, amoxicillin 500 mg orally every 8 hours is given for 7 days.
Although most perforations close spontaneously, surgery is indicated for a perforation persisting > 2 months. Persistent conductive hearing loss suggests disruption of the ossicular chain, necessitating surgical exploration and repair.
.